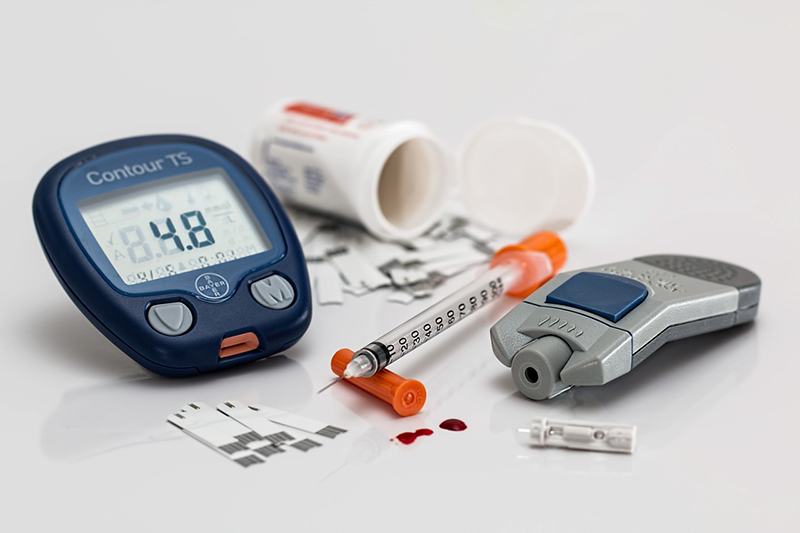
Diabetes is a lifelong, metabolic disease in which the body cannot properly store and use sugar. Diabetes is characterized by extremely high blood sugar levels, and over time, the condition can weaken the heart, injure the blood vessels, and damage the eyes, kidneys, and nervous system.
Over the past three decades, the number of people living with diabetes worldwide has increased fourfold. More than 29 million people in the United States have diabetes including almost 12 million adults aged 65 and older.
According to Wendy C. Huhn, M.D., F.A.C.E., a board-certified clinical endocrinologist at the Diabetes and Endocrine Center of Orlando, although they both share the problem of high blood sugar levels, type 1 and type 2 diabetes are not the same disease.
“Type 1 diabetes is often seen in younger people below the age of 20 and is caused by an autoimmune condition,†says Dr. Huhn. “Type 2 diabetes typically begins in adulthood. Before the onset of type 2 diabetes, a person is generally going through several years of insulin resistance and impaired glucose tolerance.â€
What Is Type 1 Diabetes?
Type 1 diabetes is a condition where the pancreas stops producing insulin. Insulin is a hormone which your body needs to enable sugar (glucose) to enter your cells to produce energy. Specific factors may contribute to diabetes including:
- Genetics
- A family history of diabetes
- Specific viruses
Type 1 diabetes most often manifests in children between 4-7 years of age or adolescents; however, it can also develop in adults. Symptoms of type 1 diabetes can come on suddenly and include:
- Increased thirst
- Frequent urination
- Sudden bed-wetting in children
- Severe hunger
- Unintended weight loss
- Irritability and other mood swings
- Fatigue and weakness
- Blurry vision
“In type 1 diabetes, the immune system starts to recognize the beta cells within the pancreas that produce insulin as something foreign,†says Dr. Huhn. “And (your system) destroys those beta cells over time, and they become unable to produce insulin. Insulin is the key to the body to open up the tissues and allow fuel to get inside our muscles, organs, and fat cells.â€
“Type 1 diabetes develops after there’s insulin deficiency,†Dr. Huhn continues. “You need to lose about 80% of your pancreas’ ability to make insulin, and without insulin, you start to break down fat, because the body isn’t able to use glucose. And fat can then release fatty acids, which are acidic, so you can get very sick if you don’t have insulin in your body.â€
If the acidic buildup in the body gets out of control, it can be life-threatening. Your body will become unable to process any glucose and will then react like it is starved for energy. Replacing insulin is the key to get things back on track. Despite active research, there remains no cure for type 1 diabetes. Treatment focuses on managing blood sugar levels with insulin, diet, and lifestyle to prevent complications.
“There are many ways of taking insulin,†says Dr. Huhn. “There are different regimens, anywhere from doing one to four shots of insulin every day, or the high tech way these days, is with insulin pump therapy. And that gives you a continuous infusion of insulin just under the skin.â€
What Is Type 2 Diabetes?
Type 2 diabetes is the most common form of diabetes mellitus and is influenced by advancing age, obesity, sedentary lifestyle, and family history. With type 2 diabetes, your pancreas produces relatively normal amounts of insulin; however, your body is unable to use the insulin effectively. As a consequence, blood sugar control is abnormal due primarily to insulin resistance.
“Insulin is the key to open up doors to the cells and tissues of the body,†says Dr. Huhn. “People with type 2 diabetes have plenty of insulin for many years. It starts to wane in its effectiveness because those keys stop fitting into the doors and the keyholes – the tissues of the body. Often people with type 2 diabetes have heredity to develop insulin resistance, or in our country, have a plethora of carbohydrates and calories that are so easily accessible.â€
“When a person develops a lot of belly fat, that fat is quite inflammatory and can also result in insulin resistance,†Dr. Huhn continues. “Over time, the insulin resistance can cause insulin deficiency because the pancreas has to overproduce so much insulin that the beta cells that produce insulin get a little burned out. They get tired. At that point, we can see the markers for diabetes, like the hemoglobin A1C and fasting glucose levels rise quite significantly.â€
How Does Type 2 Diabetes Manifest in the Body?
According to Dr. Huhn, type 2 diabetes can come about through numerous deficiencies in the body. “We find that there are at least eight areas of the body that could have defects that cause type 2 diabetes,†she says.
The Liver:
If the liver is not getting enough insulin, it will start to overproduce sugar. One of the functions of our liver is to store sugar that’s in excess and release it during times of emergency. The amount of sugar it releases is regulated by insulin. “If the liver is resistant to insulin, it will do its own thing,†says Dr. Huhn. “Often we see higher blood sugars in the morning because the effect of insulin on the liver is defective.â€
The Pancreas:
The pancreas can also be a source for type 2 diabetes. Beta cells within the islet cells in the pancreas produce insulin. A defect in the pancreas’ ability to produce insulin will cause problems. Other cells within the pancreas, called alpha cells, can overproduce an anti-insulin hormone called glucagon.
“Glucagon, when we eat, should be suppressed, and that allows the insulin to work better,†says Dr. Huhn. “In type 2 diabetes, we often see an elevation in glucagon after eating. That makes it harder for insulin to work properly. Muscles or fat cells can also become resistant to insulin over time. The keys aren’t working to open up those cells to allow the fuel to run our muscles or to store our extra calories and fat properly. When that happens, the sugar spikes in the bloodstream.â€
The Kidneys, GI Tract, and the Brain:
The kidneys can also be the origin for diabetes defect. There are enzymes in the kidneys that are supposed to release extra sugar into the urine. But the abnormality causes the sugar to be reabsorbed back into the bloodstream, rather than being eliminated.
The gastrointestinal tract can be problematic when it forgets how to make incretins – hormones from the gut that tells the pancreas to release insulin, suppress glucagon and slow down how fast you’re absorbing glucose from your food. The brain can be defective in type 2 diabetes as it doesn’t realize that you’re already full, and you end up overeating.
Treatments for Type 2 Diabetes
 Depending on which deficiency has led to the manifestation of type 2 diabetes, different treatment modalities exist to address it.
Depending on which deficiency has led to the manifestation of type 2 diabetes, different treatment modalities exist to address it.
“Medications to treat the different abnormalities depend on what the defect is,†says Dr. Huhn. “If the liver releases too much sugar, we use Metformin to try to eliminate that. When the pancreas isn’t making insulin, we use insulin or sulfonylureas like Glipizide that cause the beta cells to release extra insulin.â€
“The alpha cell difficulty, if that is not being suppressed, and it’s making glucagon when we eat, medications classified as DPPP-4 inhibitors and GLP-1 agonists, like Januvia and Victoza are used. SGLT2 inhibitors like Invokana, Farxiga, or Jardiance are used to suppress the reabsorption of sugar back into the bloodstream by the kidneys. With the gut, to get those hormones back up to normal, we use the GLP-1s and the DPPP-4s also. And we also use GLP receptor agonists to tell the brain ‘yes, we are full.’â€
Dr. Huhn notes that diabetes can start with one defect, and then more deficiencies may appear later on. “Patients may start with one or two medications and have to add or change their regimen as time goes on,†she says. “The main goal is to reduce the average blood sugar so that A1C levels are between 6% and 7%.â€



Leave A Comment